Diabetic Retinopathy

Diabetic retinopathy, the most common diabetic eye disease, occurs when blood vessels in the retina change. Sometimes these vessels swell and leak fluid or even close off completely. In other cases, abnormal new blood vessels grow on the surface of the retina.
The retina is a thin layer of light-sensitive tissue that lines the back of the eye. Light rays are focused onto the retina, where they are transmitted to the brain and interpreted as the images you see. The macula is a very small area at the center of the retina. It is the macula that is responsible for your pinpoint vision, allowing you to read, sew or recognize a face. The surrounding part of the retina, called the peripheral retina, is responsible for your side—or peripheral—vision.
Diabetic retinopathy usually affects both eyes. People who have diabetic retinopathy often don’t notice changes in their vision in the disease’s early stages. But as it progresses, diabetic retinopathy usually causes vision loss that in many cases cannot be reversed.
Diabetic eye problems
There are two types of diabetic retinopathy:
Background or nonproliferative diabetic retinopathy (NPDR)
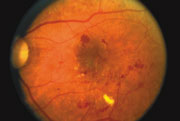
Nonproliferative diabetic retinopathy (NPDR) is the earliest stage of diabetic retinopathy. With this condition, damaged blood vessels in the retina begin to leak extra fluid and small amounts of blood into the eye. Sometimes, deposits of cholesterol or other fats from the blood may leak into the retina.
NPDR can cause changes in the eye, including:
- Microaneurysms: small bulges in blood vessels of the retina that often leak fluid.
- Retinal hemorrhages: tiny spots of blood that leak into the retina.
- Hard exudates: deposits of cholesterol or other fats from the blood that have leaked into the retina.
- Macular edema: swelling or thickening of the macula caused by fluid leaking from the retina’s blood vessels. The macula doesn’t function properly when it is swollen. Macular edema is the most common cause of vision loss in diabetes.
- Macular ischemia: small blood vessels (capillaries) close. Your vision blurs because the macula no longer receives enough blood to work properly.
Many people with diabetes have mild NPDR, which usually does not affect their vision. However, if their vision is affected, it is the result of macular edema and macular ischemia.
Proliferative diabetic retinopathy (PDR)
Proliferative diabetic retinopathy (PDR) mainly occurs when many of the blood vessels in the retina close, preventing enough blood flow. In an attempt to supply blood to the area where the original vessels closed, the retina responds by growing new blood vessels. This is called neovascularization. However, these new blood vessels are abnormal and do not supply the retina with proper blood flow. The new vessels are also often accompanied by scar tissue that may cause the retina to wrinkle or detach.
PDR may cause more severe vision loss than NPDR because it can affect both central and peripheral vision. PDR affects vision in the following ways:
Vitreous hemorrhage: delicate new blood vessels bleed into the vitreous — the gel in the center of the eye — preventing light rays from reaching the retina. If the vitreous hemorrhage is small, you may see a few new, dark floaters. A very large hemorrhage might block out all vision, allowing you to perceive only light and dark. Vitreous hemorrhage alone does not cause permanent vision loss. When the blood clears, your vision may return to its former level unless the macula has been damaged.
Traction retinal detachment: scar tissue from neovascularization shrinks, causing the retina to wrinkle and pull from its normal position. Macular wrinkling can distort your vision. More severe vision loss can occur if the macula or large areas of the retina are detached.
Neovascular glaucoma: if a number of retinal vessels are closed, neovascularization can occur in the iris (the colored part of the eye). In this condition, the new blood vessels may block the normal flow of fluid out of the eye. Pressure builds up in the eye, a particularly severe condition that causes damage to the optic nerve.
Diabetic Retinopathy Diagnosis
The only way to detect diabetic retinopathy and to monitor its progression is through a comprehensive eye exam.
There are several parts to the exam:
Visual acuity test
This uses an eye chart to measure how well you can distinguish object details and shape at various distances. Perfect visual acuity is 20/20 or better. Legal blindness is defined as worse than or equal to 20/200 in both eyes.
Slit-lamp exam
A type of microscope is used to examine the front part of the eye, including the eyelids, conjunctiva, sclera, cornea, iris, anterior chamber, lens, and also parts of the retina and optic nerve.
Dilated exam
Drops are placed in your eyes to widen, or dilate, the pupil, enabling your Eye M.D. to examine more thoroughly the retina and optic nerve for signs of damage.
It is important that your blood sugar be consistently controlled for several days when you see your eye doctor for a routine exam. If your blood sugar is uneven, causing a change in your eye’s focusing power, it will interfere with the measurements your doctor needs to make when prescribing new eyeglasses. Glasses that work well when your blood sugar is out of control will not work well when your blood sugar level is stable.
Your Eye M.D. may find the following additional tests useful to help determine why vision is blurred, whether laser treatment should be started, and, if so, where to apply laser treatment.
Fluorescein angiography
Your doctor may order fluorescein angiography to further evaluate your retina or to guide laser treatment if it is necessary. This is a diagnostic procedure that uses a special camera to take a series of photographs of the retina after a small amount of yellow dye (fluorescein) is injected into a vein in your arm. The photographs of fluorescein dye traveling throughout the retinal vessels show:
- Which blood vessels are leaking fluid;
- How much fluid is leaking;
- How many blood vessels are closed;
- Whether neovascularization is beginning.
Optical coherence tomography (OCT)
OCT is a non-invasive scanning laser that provides high-resolution images of the retina, helping your Eye M.D. evaluate its thickness. OCT can provide information about the presence and severity ofmacular edema (swelling).
Ultrasound
If your ophthalmologist cannot see the retina because of vitreous hemorrhage, an ultrasound test may be done in the office. The ultrasound can “see” through the blood to determine if your retina has detached. If there is detachment near the macula, this often calls for prompt surgery.
When your diabetic retinopathy screening is complete, your ophthalmologist will decide when you need to be treated or re-examined.
If you have diabetes, you should see your ophthalmologist right away if you have any visual changes that affect only one eye, last more than a few days, and are not associated with a change in blood sugar.
When to schedule an eye examination
Diabetic retinopathy usually takes years to develop, which is why it is important to have regular eye exams. Because people with Type 2 diabetes may have been living with the disease for some time before they are diagnosed, it is important that they see an ophthalmologist (Eye M.D.) without delay.
The American Academy of Ophthalmology recommends the following diabetic eye screening schedule for people with diabetes:
Type 1 Diabetes: Within five years of being diagnosed and then yearly.
Type 2 Diabetes: At the time of diabetes diagnosis and then yearly.
During pregnancy: Pregnant women with diabetes should schedule an appointment with their ophthalmologist in the first trimester because retinopathy can progress quickly during pregnancy.
Diabetic Retinopathy Treatment
The best treatment for diabetic retinopathy is to prevent it. Strict control of your blood sugar will significantly reduce the long-term risk of vision loss. Treatment usually won’t cure diabetic retinopathy nor does it usually restore normal vision, but it may slow the progression of vision loss. Without treatment, diabetic retinopathy progresses steadily from minimal to severe stages.
Laser surgery
The laser is a very bright, finely focused light. It passes through the clear cornea, lens and vitreous without affecting them in any way. Laser surgery shrinks abnormal new vessels and reduces macular swelling. Treatment is often recommended for people with macular edema, proliferative diabetic retinopathy (PDR) and neovascular glaucoma.
Laser surgery is usually performed in an office setting. For comfort during the procedure, an anesthetic eyedrop is often all that is necessary, although an anesthetic injection is sometimes given next to the eye. The patient sits at an instrument called a slit-lamp microscope. A contact lens is temporarily placed on the eye in order to focus the laser light on the retina with pinpoint accuracy.
A few people may see laser spots near the center of their vision following treatment. They usually fade with time, but may not disappear completely.
In PDR, the laser is applied to all parts of the retina except the macula (called PRP, or panretinal photocoagulation). This treatment causes abnormal new vessels to shrink and often prevents them from growing in the future. It also decreases the chance that vitreous bleeding or retinal distortion will occur. Panretinal laser has proven to be very effective for preventing severe vision loss from vitreous hemorrhage and traction retinal detachment.
Multiple laser treatments over time may be necessary. Laser surgery does not cure diabetic retinopathy and does not always prevent further loss of vision.
Vitrectomy surgery
Vitrectomy is a surgical procedure performed in a hospital or ambulatory surgery center operating room. It is often performed on an outpatient basis or with a short hospital stay. Either a local or general anesthetic may be used.
During vitrectomy surgery, an operating microscope and small surgical instruments are used to remove blood and scar tissue that accompany abnormal vessels in the eye. Removing the vitreous hemorrhage allows light rays to focus on the retina again.
Vitrectomy often prevents further vitreous hemorrhage by removing the abnormal vessels that caused the bleeding. Removal of the scar tissue helps the retina return to its normal location. Laser surgery may be performed during vitrectomy surgery. To help the retina heal in place, your ophthalmologist may place a gas or oil bubble in the vitreous space. You may be told to keep your head in certain positions while the bubble helps to heal the retina. It is important to follow your ophthalmologist’s instructions so your eye will heal properly.
Medication injections
In some cases, medication may be used to help treat diabetic retinopathy. Sometimes a steroid medication is used. In other cases, you may be given an anti-VEGF medication. This medication works by blocking a substance known as vascular endothelial growth factor, or VEGF. This substance contributes to abnormal blood vessel growth in the eye which can affect your vision. An anti-VEGF drug can help reduce the growth of these abnormal blood vessels.
After your pupil is dilated and your eye is numbed with anesthesia, the medication is injected into the vitreous, or jelly-like substance in the back chamber of the eye. The medication reduces the swelling, leakage, and growth of unwanted blood vessel growth in the retina, and may improve how well you see.
Medication treatments may be given once or as a series of injections at regular intervals, usually around every four to six weeks or as determined by your doctor.
Who Is at Risk for Diabetic Retinopathy?
People with diabetes are at risk for developing diabetic retinopathy. Diabetes is a disease that affects the body’s ability to produce or use insulin effectively to control blood sugar levels.
There are three types of diabetes.
- Type 1 diabetes: usually diagnosed in children and young adults and previously known as juvenile diabetes, where the body does not produce insulin.
- Type 2 diabetes: the most common form of diabetes. Either the body does not produce enough insulin or the body’s cells ignore the insulin.
- Gestational diabetes: blood sugar levels (glucose) become elevated during pregnancy in women who have never had diabetes before. Gestational diabetes starts when the mother’s body is not able to make and use all the insulin it needs during pregnancy.
People with any type of diabetes can develop hyperglycemia, which is an excess of blood sugar, or serum glucose. Although glucose is a vital source of energy for the body’s cells, a chronic elevation of serum glucose causes damage throughout the body, including the small blood vessels in the eyes.
Diabetic retinopathy risk factors
Several factors can influence the development and severity of diabetic retinopathy, including:
- Blood sugar levels
Controlling your blood sugar is the key risk factor that you can affect. Lower blood sugar levels can delay the onset and slow the progression of diabetic retinopathy. - Blood pressure
A major clinical trial demonstrated that effectively controlling blood pressure reduces the risk of retinopathy progression and visual acuity deterioration. High blood pressure damages your blood vessels, raising the chances for eye problems. Target blood pressure for most people with diabetes is less than 130/80 mmHg. - Duration of diabetes
The risk of developing diabetic retinopathy or having your disease progress increases over time. After 15 years, 80 percent of Type 1 patients will have diabetic retinopathy. After 19 years, up to 84 percent of patients with Type 2 diabetes will have diabetic retinopathy. - Blood lipid levels (cholesterol and triglycerides)
Elevated blood lipid levels can lead to greater accumulation of exudates, protein deposits that leak into the retina. This condition is associated with a higher risk of moderate visual loss. - Ethnicity
While diabetic retinopathy can happen to anyone with diabetes, certain ethnic groups are at higher risk because they are more likely to have diabetes. These include African Americans, Latinos and Native Americans. - Pregnancy
Being pregnant can cause changes to your eyes. If you have diabetes and become pregnant, your risk for diabetic retinopathy increases. If you already have diabetic retinopathy, it may progress. However, some studies have suggested that with treatment these changes are reversed after you give birth and that there is no increase in long-term progression of the disease.
